2–4%
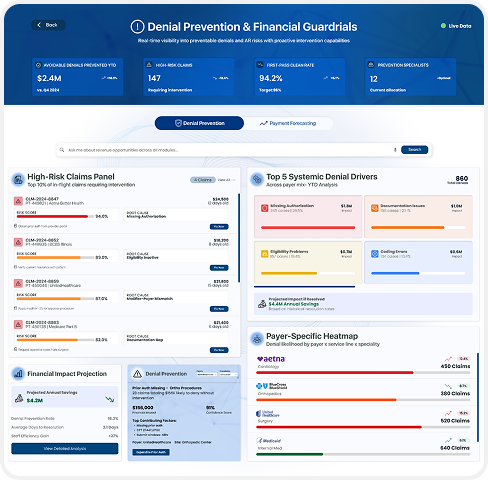
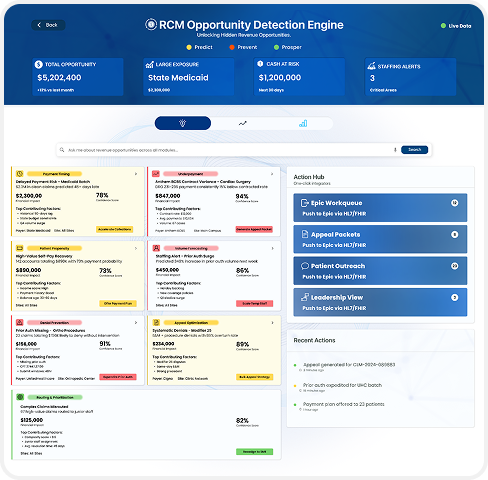
Our recovery engine connects directly to your existing systems, continuously ingesting claims, remit, contract, and payer data. It detects where revenue is at risk, predicts which accounts will impact margin next, and automatically routes the right actions to your teams, before revenue is actually lost.
Unlike traditional analytics tools that surface issues after write-offs have occurred, this system gives you foresight and activation. Every insight is tied to dollar value, ranked by recovery probability, and pushed into your operational workflows in real time.
A Proactive Recovery System Built for Continuous Financial Impact
Even with strong teams and established systems, financial losses continue because traditional RCM tools surface issues too late; once revenue has been delayed, or worse, already written off.
Even with strong teams and established systems, financial losses continue because traditional RCM tools surface issues too late; once revenue has been delayed, or worse, already written off.
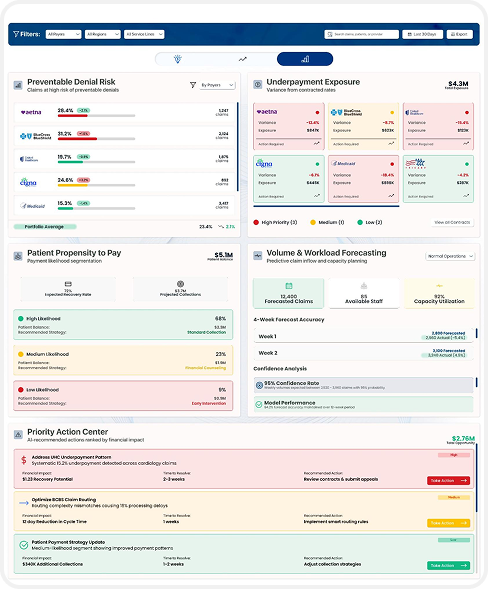
You know underpayments are occurring, but you lack contract-level visibility across payers to identify and recover variance at scale.
Your teams are working claims, yet revenue impact remains unclear because actions aren’t prioritized by financial value or probability of recovery.
You rely on retrospective reports rather than forward-looking intelligence, forcing you to react to preventable revenue loss after it has already occurred, instead of intervening ahead of the curve.
We combine deep revenue cycle expertise with advanced machine learning architecture to deliver a proactive recovery engine built exclusively for the needs of healthcare teams.
Even with strong teams and established systems, financial losses continue because traditional RCM tools surface issues too late; once revenue has been delayed, or worse, already written off.
We push prioritized actions directly into Epic, Cerner, and your operational work queues, so your teams execute within their existing systems, without disruption.
Net Patient Revenue uplift
First-Pass Yield and denial prevention
A/R days and cash acceleration
Underpayment recovery rates
Cost-to-collect reduction
The opportunity detection engine is calibrated to your payer mix, contract rules, service lines, and staffing model so the engine works how your organization operates, not the other way around. The customised solution stack resides securely within your enterprise architecture
Our models learn from your performance over time, continuously identifying unrealized revenue and tracking every action to financial realization. Value compounds, month after month.

An analysis of unrealized revenue across denials, underpayments, and patient responsibility
A personalized roadmap powered by your payer mix and contract terms
Recommendations tailored to your operating model, teams, and financial goals
The revenue is already in your system. We help you capture it, before it’s lost.

