Billing offices for large healthcare groups often face heavy workloads. Encoda’s integrated billing tools have changed this for a 130-provider group. These tools increased staff productivity by 30%, helping teams manage their tasks better. This improvement came from automation, as shown by the 130-provider group’s experience.
The Challenge of Growing Billing Workloads
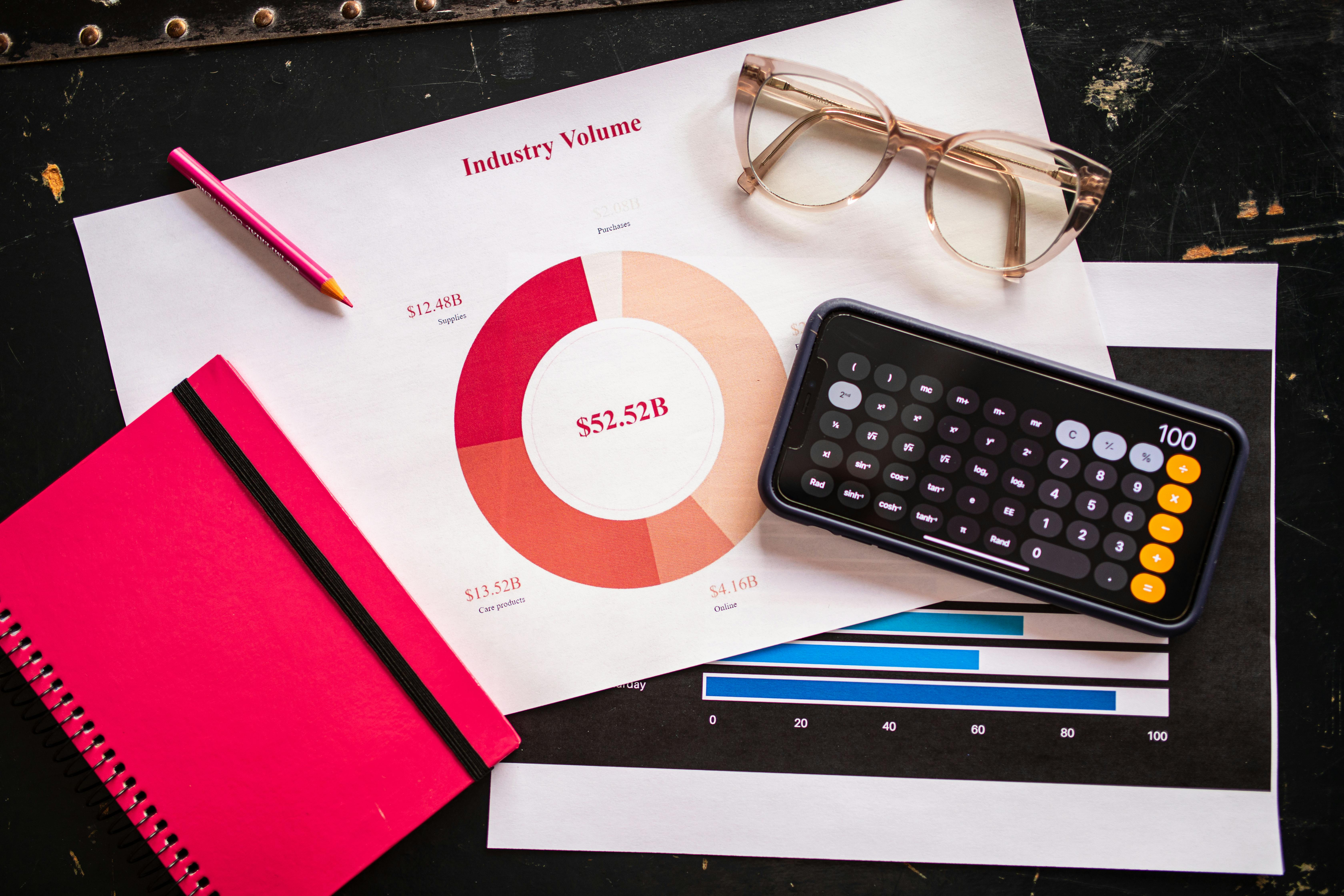
Managing billing for 130 providers puts pressure on any team. In the past, staff handled claims and denials manually, following payer rules. This led to tiredness and mistakes. In 2024, inefficient workflows cost healthcare systems $12 billion annually, with staff spending 30% of their time on routine tasks. Without new tools, this was a common problem.
As the number of providers grows, coordinating clearinghouses, EHRs, and payer systems becomes harder. Key issues include:
- Time lost switching between systems
- Payment disputes slowing work
- Errors delaying payments
For a 130-provider group, this inefficiency threatened financial stability, creating a need for scalable solutions without adding staff.
Encoda’s Effective Workflow Solution
Encoda’s integrated billing tools bring all workflows into one platform. By connecting insurance portals, EHRs, and clearinghouses, Encoda improves efficiency. A 130-provider group with a 12-person team saw clear benefits. Automation managed tasks like claim checks and payment tracking, reducing staff workload.
The tools simplify daily work. Adjusting patient accounts or tracking payer changes, once time-consuming, now run smoothly. This allowed staff to focus on important tasks, such as insurer talks or provider advice. After 50 days, productivity rose by 30%, thanks to healthcare analytics that turns data into useful insights.
Real Results: A Team’s Improvement
Look at the 130-provider group’s experience, a strong example of Encoda’s impact. Before the tools, their 12 staff struggled with scattered workflows, spending days on manual fixes instead of revenue work. With Encoda’s platform, they reduced their claims team from five to four while still covering all 130 providers.
This gain comes from healthcare analytics that identifies issues early. Encoda’s real-time dashboard showed financial status, helping staff prioritize urgent claims. The team reported higher productivity with fewer resources. Industry data supports this, with automation cutting operational costs by 20-30% in revenue tasks. This saved hours weekly, changing how the team works.
A similar 128-provider group also improved, reducing manual work by 25% with Encoda’s help, focusing on patient care. This shows how healthcare analytics enhances efficiency for others.
How Automation Supports This Success
Automation is key to Encoda’s success. It handles repetitive tasks, easing staff pressure and allowing strategic focus. For the 130-provider team, automated alerts caught payment errors quickly, cutting review time by 40%. This connects to advanced data analysis, where claim patterns guide decisions.
Accuracy is important in healthcare. Errors in submissions can delay payments, affecting finances. Encoda’s tools check claims against payer rules, finding issues early. This led to fewer denials and faster revenue for the 130-provider group, improving cash flow.
Also, healthcare analytics offers predictive insights. By analyzing past data, Encoda spots potential workflow issues, enabling proactive adjustments. This kept the 130-provider team efficient as demands grew.
Benefits Beyond Productivity
Encoda’s tools provide more than just efficiency gains. Staff move to meaningful tasks, improving morale in a challenging industry. Providers benefit from faster workflows, supporting better care. The 130-provider group saw a 15% morale increase with their productivity rise.
Healthcare analytics gives leaders clear insights. Dashboards show payer trends and team performance, aiding resource planning. This approach, like healthcare data analytics services, helped the 130-provider team maintain a small staff.
Financially, efficient management of 130 providers recovered lost revenue, matching $18 billion in potential automation savings. This wide impact makes Encoda’s tools essential for large operations.
Frequently Asked Questions
How Does Encoda Help During Staff Absences?
Encoda’s automation ensures work continues smoothly, covering tasks when staff are unavailable.
What Technical Support Does Encoda Offer?
Encoda provides 24/7 technical assistance, ensuring quick resolution of any system issues.
How Does Encoda Manage Large Data Volumes?
Encoda uses efficient data processing to handle high volumes, maintaining performance for 130 providers.
Can Encoda Assist with Staff Performance Reviews?
Yes, Encoda offers analytics to track individual contributions, supporting fair performance evaluations.
How Does Encoda Ensure System Uptime?
Encoda maintains robust servers with regular updates, minimizing downtime for continuous operation.
Can Integrated Tools Improve Healthcare Efficiency?
Integrated tools like Encoda’s show potential to enhance healthcare efficiency. Their success with a 130-provider group, boosting productivity by 30% and improving morale, demonstrates clear benefits. This approach reduces costs and streamlines operations, offering a model for other healthcare organizations. The use of healthcare analytics provides data-driven insights that support better decision-making and resource use. As the industry seeks ways to optimize workflows, such tools could set a new standard. Their ability to handle large provider networks without adding staff highlights scalability. This evidence suggests a promising future for healthcare efficiency.
Contact Ascend Analytics for a FREE strategy session to explore healthcare analytics consulting and see how it can benefit your practice!